Author Archives: Stewart Mercer
The CARE Plus study
ABC of multimorbidity
Tweet
By Stewart Mercer, Chris Salisbury and Martin Fortin
The ABC of multimorbidity is a book (64 pages) recently published by WILEY Blackwell seeking to explore some important issues on the subject. Contributors to the book were Marjan van den Akker, Elizabeth A. Bayliss, Peter Bower, Sonny Cejic, Peter Coventry, Martin Fortin, Katie I. Gallacher, Linda Gask, Jane Gunn, Karen Kinder, Frances Mair, Carl May, Stewart W. Mercer, Victor Montori, Christiane Muth, Ignacio Ricci-Cabello, Martin Roland, Chris Salisbury, Efrat Shadmi, Moira Stewart, Amanda L. Terry, José M. Valderas, Concepción Violán, and Jonathan P. Weiner.
Divided in 12 chapters, the book addresses the prevalence of multimorbidity, its impact on patients, the relationship between physical and mental health problems, and how managing multiple health problems concurrently can create a heavy burden of treatment for patients. At the heart of the book is the authors’ shared conviction that health care should be person -centered.
Due to space limitations each chapter is rather short. We hope that experts on the subject do not judge us too severely for the limited amount of information we could provide, and that busy physicians looking for an informative and practical source of knowledge will find this book useful.
Can we exclude exclusion criteria?
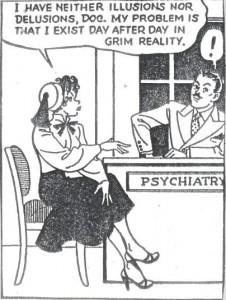
I keep a cartoon in which a patient tells a flummoxed psychiatrist,
” I have neither illusions nor delusions, Doc. My problem is that I exist day after day in grim reality”.
In seeking to pigeon-hole the patient as a case, the doctor ignores her reality.
Does the same thing happen in multiple morbidity?
Shakespeare first noted, “When troubles come, they come not single spies but in batallions”
That seems true of multiple morbidity in socio-economically deprived areas, defined as the “number, severity and complexity of health and social problems within families”.
Operational definitions of multiple morbidity in research studies, based on counts of conditions, get nowhere near this, largely missing out on social and family aspects.
The problem is heterogenity, something that research tries to eliminate.
How can multiple morbidity research put heterogenity centre stage, so that results inform the majority of patients’ circumstances and not only those meeting case definitions?
Of course, asking the question is the easy part.
International Workshop, Glasgow, April 18th, 2011
By Stewart Mercer
The challenge of multimorbidity – what can we learn from cohort studies?
This one day meeting was organised by Professor Stewart Mercer, Professor of Primary Care Research at the University of Glasgow, who leads a national research programme on multimorbidity in Scotland with the Scottish School of Primary Care.
The morning seminar, which was the inaugural event of the newly established Institute of Health and Well-being at the University of Glasgow, and was chaired by Professor Sally Wyke, welcomed Professor Jane Gunn from Melbourne University, who is Visiting Professor with the Scottish School of Primary Care, who described her work over several years on the DIAMOND primary care cohort on depression and multimorbidity. Professor Martin Fortin from Sherbrooke University in Canada, then described the cohort studies he has recently been involved in setting up in primary care in Canada with Professor Jeannie Haggerty. This was followed by Professor Frances Mair, Head of the Academic Unit of General Practice and Primary Care at the University of Glasgow, who spoke of the treatment burden in multimorbidity, and the need for ‘minimally disruptive medicine.’ Finally, Professor Mercer described work to date on multimorbidity in Scotland, and work in progress in developing the MALT (Multiple and Long-Term conditions) cohort in Scotland.
The afternoon consisted of a workshop to discuss multimorbidity cohort studies further, and the MALT Cohort development. Attendees included experts from Scotland, Ireland, England, as well as our morning speakers. The need for cohort studies on multimorbidity was agreed, based on simple models, and as far as possible based on collaboration between countries. The lack of evidence on multimorbid patients’ views and experiences of health and healthcare was a strong theme of the afternoon. It was agreed that those at the workshop would continue to debate these issues collaboratively.
Overall, this was a very enjoyable and stimulating meeting and we look forward to seeing more guests in the future at our next ‘Glasgow Meeting’ on interventions in multimorbidity in March next year.