Author Archives: Administrator
Appreciation of Dr. Martin Fortin’s work on multimorbidity
‘Addressing the global challenge of multimorbidity’: Call for written evidence
The Academy of Medical Sciences has recently launched a new working group project on ‘Addressing the global challenge of multimorbidity’ and is seeking your views on multimorbidity as an international health challenge.
Throughout the world, as life expectancy increases, the population incidence of non-communicable diseases is also increasing. Further, communicable diseases, with both their short and long term sequelae, continue to affect millions of people every year. Together, all of these factors mean that multimorbidity has become, and will increasingly be, an international health challenge.
However, currently there is no commonly used framework for defining or more widely understanding multimorbidity. Further, most health related research is currently focused on the prevention and management of disorders in isolation. Consequently, it is difficult to compile a coherent body of research in this area or develop evidence-based strategies for use in healthcare systems. In order to address the challenge of multimorbidity, we must understand the problem better.
The questions outlined in the call for written evidence have therefore been developed to gather information on the definition(s) of multimorbidity, better understand the current knowledge base on multimorbidity as an international health challenge, and to gather opinions about future priorities and opportunities.
This call is part of our process of gathering external input into the project, and we would welcome responses from external stakeholders, including researchers, healthcare professionals, research institutions, funders, industry, patients and members of the public.
The deadline for submission is 30 November 2016.
For more information about the project and to submit a response, please visit the Academy’s website. If you have any questions, please contact Dr Rachel Brown (rachel.brown@acmedsci.ac.uk).
Conference Personalized Geriatric Medicine
Tweet
Invitation
The Swedish Society of Medicine is inviting to a 3-day international conference called “Personalized Geriatric Medicine”, in Stockholm/Sweden August 20-22, 2014. The conference is arranged in collaboration with the Swedish Society for Geriatric Medicine, European Union Geriatric Medicine Society (EUGMS), Karolinska Institutet and The Swedish Research Council.
The program will focus on management of individual frail, multimorbid elderly people over time in relation to medical quality, patient safety, education/training and research/development. World leading researchers are invited as speakers and will present state-of-the-art lectures. We aim to highlight the potential of Geriatric Medicine to improve the quality of multi-domain analysis, management/care and follow-up over time in individual multimorbid, elderly people. The potential of the medical record to serve as a much longed for “geroscope” will be highlighted. Each symposium day includes group discussions, where the participants and speakers meet to discuss various themes more personal and in-depth.
The conference is hoped to attract scientists, clinicians from different medical specialities, health care staff groups, stakeholders and others with interest in various aspects of improving health care, assessment and managment/care of multimorbid, elderly people.
For more information about the conference and how to register, please visit the conference homepage: http://www.sls.se/Utbildning/Berzeliussymposier/geriatricmedicine/.
Welcome to Stockholm in August 2014!
Stockholm, Sweden March 10, 2014
On behalf of the Organizing committee
Gunnar Akner
Chair
Professor in Geriatric Medicine, Senior physician
Looking for a consensus for a definition of multimorbidity: the results
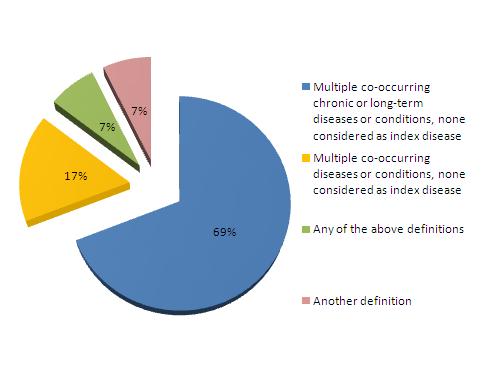
We have computed the results of the survey we conducted recently on the definition of multimorbidity.
We received 55 responses from 16 countries. The distribution of respondents by country (in alphabetic order) was: Australia 4, Brazil 1, Canada 10, China 1, Egypt 1, Germany 1, India 1, Indonesia 1, Ireland 6, Netherlands 4, South Korea 1, Spain 6, Switzerland 1, Turkey 1, United Kingdom 10 (3 of them from Scotland), United States of America 6.
Answers to the question “which definition do you think should be used for multimorbidity?” were as follows:
Comments associated with the responses to the last item are shown below as replies to this posting. We welcome more comments on this subject that can also be written as replies to the posting.
We want to thank all participants who shared their view on this subject.
The International Research Community on Multimorbidity
Comparisons of multi-morbidity in family practice – issues and biases
By Moira Stewart, Martin Fortin, Helena Britt, Christopher Harrison, and Heather Maddocks
A recent study published in Family Practice “Comparisons of multi-morbidity in family practice – issues and biases” [1] compared the methods and results of three separate prevalence studies of multi-morbidity from; i) the Saguenay region of Quebec [2]; ii) a sub-study of the Bettering Evaluation and Care of Health (BEACH) program in Australia [3,4]; and iii) the Deliver Primary Health Care Information (DELPHI) project in South-western Ontario [5,6].
A re-estimate of the prevalence rates using identical age-sex groups found multi-morbidity prevalence to vary by as much as 61%, where reported prevalence was 95% among females aged 45–64 in the Saguenay study, 46% in the BEACH sub-study and 34% in the DELPHI study.
Several aspects of the methods and study designs were identified as differing among the studies, including the sampling of frequent attenders, sampling period, source of data, and both the definition and count of chronic conditions.
The paper offers a guide for authors reporting the methods used in multi-morbidity prevalence research, recommending detailed descriptions of the type of sampling, completeness and accuracy of the source of data, and the definition of chronic conditions.
Further comparisons among multi-morbidity data using agreed upon standards for the definition of chronic conditions and the way to count multi-morbidity are recommended to assess the impact of these methodological variations.
References:
1 Stewart M, Fortin M, Britt H, Harrison C, Maddocks H. Comparisons of multi-morbidity in family practice – issues and biases. Family Practice. May 2013. doi: 10.1093/fampra/cmt012.
2 Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med 2005; 3: 223–8.
3 Britt HC, Harrison CM, Miller GC, Knox SA. Prevalence and patterns of multimorbidity in Australia. Med J Aust 2008; 189: 72–7.
4 Knox SA, Harrison CM, Britt HC, Henderson JV. Estimating prevalence of common chronic morbidities in Australia. Med J Aust 2008; 189: 66–70.
5 Stewart M, Thind A, Terry AL, et al. Multimorbidity in primary care: a study using electronic medical record (EMR) data. In: Thirty-Seventh Annual Meeting of North American Primary Care Research Group, Quebec, Canada, 14–18 November, 2009.
6 Stewart M, Thind A, Terry A, Chevendra V, Marshall JN. Implementing and maintaining a researchable database from electronic medical records—a perspective from an academic family medicine department. Healthc Policy 2009; 5: 26–39.